The journey from groundbreaking laboratory discoveries to tangible healthcare solutions remains one of modern medicine’s most challenging obstacles, demanding innovative approaches and collaborative frameworks. 🔬
Understanding the Translational Research Landscape
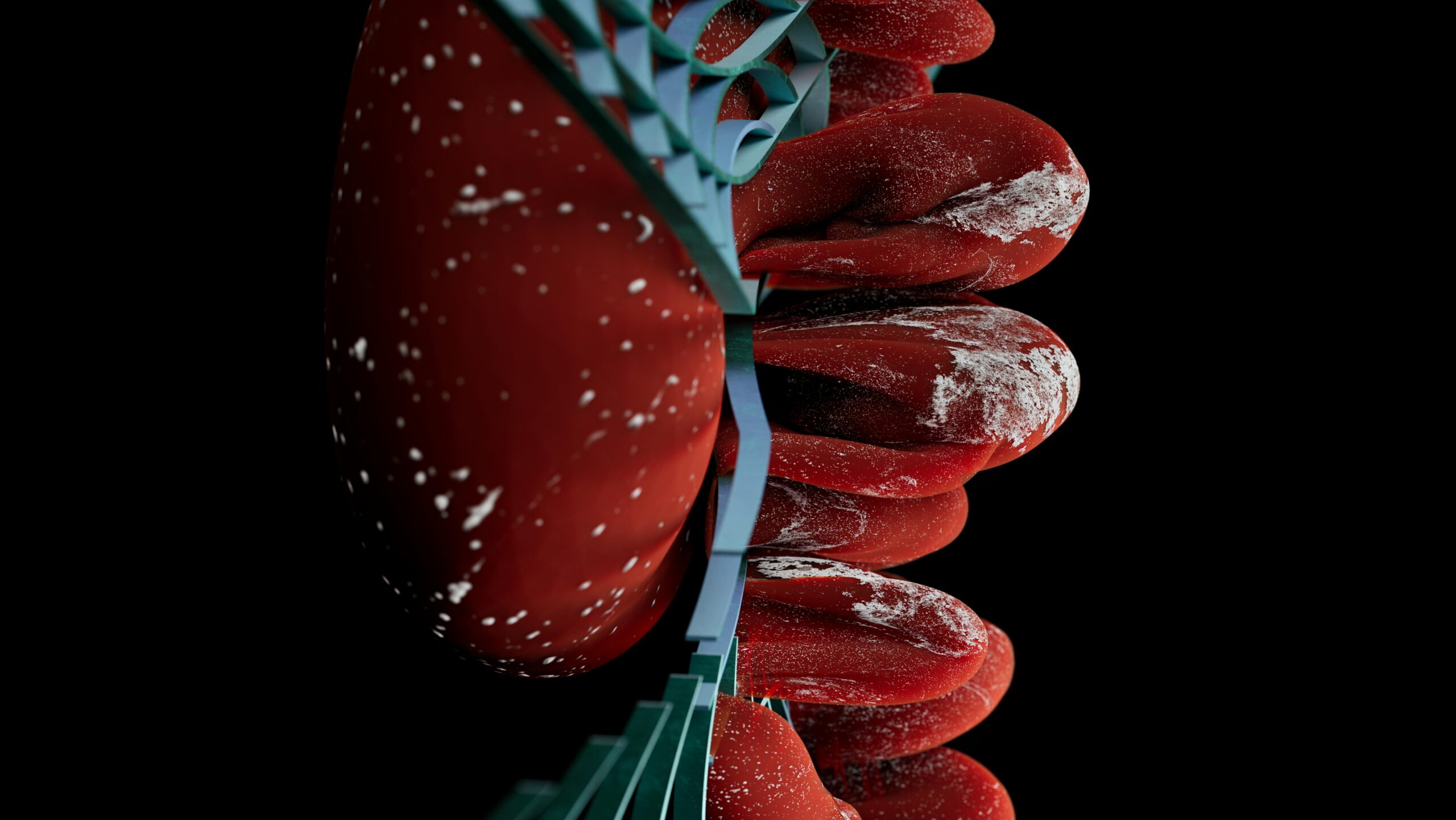
Translational research represents the critical bridge connecting basic science discoveries with clinical applications that directly benefit patients. This multidisciplinary approach seeks to transform laboratory findings into diagnostics, therapeutics, and preventive strategies that address real-world health challenges.
The traditional research pipeline often experiences significant delays between initial discovery and clinical implementation. Studies suggest that it takes an average of 17 years for research evidence to reach clinical practice, with only 14% of original discoveries eventually making it to patient care. This gap represents not just lost time, but missed opportunities to improve health outcomes and save lives.
The complexity of translational research stems from multiple factors including regulatory requirements, funding limitations, lack of interdisciplinary collaboration, and the inherent challenges of scaling laboratory findings to diverse patient populations. Addressing these barriers requires systematic changes across the entire research ecosystem.
The Valley of Death: Where Promising Research Goes to Die 💀
One of the most significant obstacles in translational research is the so-called “valley of death” – the challenging transition phase between proof-of-concept and commercial viability. This critical juncture claims numerous potentially transformative discoveries that fail to secure sufficient funding or institutional support to progress forward.
During this phase, researchers face substantial challenges in demonstrating clinical relevance, establishing manufacturing feasibility, and attracting investment for further development. The risk profile increases dramatically, and traditional funding sources often hesitate to commit resources without clear evidence of commercial potential or clinical efficacy.
Biotechnology startups frequently struggle during this period, lacking the infrastructure and resources of established pharmaceutical companies while facing the enormous costs associated with preclinical and clinical development. Many promising therapeutic candidates never reach patients simply because they cannot navigate this treacherous terrain.
Financial Barriers and Funding Gaps
The financial landscape of translational research presents formidable challenges. Basic research typically receives government funding through grants, while late-stage clinical trials attract private investment. However, the middle stages often fall into a funding gap where neither public nor private sources are willing to take the risk.
This funding chasm particularly affects academic researchers who lack the business expertise and connections to attract venture capital or pharmaceutical partnerships. Innovative financing models, including translational research centers, proof-of-concept funds, and public-private partnerships, are emerging to address this critical need.
Building Bridges Through Collaborative Frameworks 🌉
Successful translational research increasingly depends on robust collaborative networks that bring together diverse expertise. Academic institutions, healthcare systems, industry partners, and patient advocacy groups must work in concert to accelerate the translation of discoveries into practical applications.
Interdisciplinary teams that combine basic scientists, clinical researchers, regulatory experts, and business development professionals create synergies that individual researchers cannot achieve alone. These collaborations facilitate knowledge exchange, resource sharing, and the integration of multiple perspectives essential for navigating the complex translational pathway.
Academic medical centers have established translational research programs that create institutional frameworks supporting this collaborative approach. These programs provide infrastructure, expertise, and coordination mechanisms that help researchers overcome traditional silos and accelerate progress toward clinical applications.
The Role of Clinical and Translational Science Awards
The National Institutes of Health Clinical and Translational Science Awards (CTSA) program exemplifies systematic efforts to strengthen translational research infrastructure. This network of academic health centers provides resources, training, and support specifically designed to accelerate the translational process.
CTSA hubs offer services including regulatory support, biostatistics consultation, community engagement expertise, and access to innovative clinical research designs. By consolidating these resources, the program reduces barriers that individual researchers would otherwise face when attempting to translate their discoveries.
Regulatory Pathways: Navigating the Approval Maze 📋
Regulatory requirements represent both essential safeguards and significant hurdles in translational research. Understanding and efficiently navigating regulatory pathways can dramatically accelerate the journey from laboratory to clinic while maintaining appropriate safety and efficacy standards.
Regulatory agencies worldwide have recognized the need for more flexible and adaptive approaches to reviewing innovative therapies. Accelerated approval pathways, breakthrough therapy designations, and adaptive trial designs offer mechanisms for faster evaluation of promising treatments while preserving patient safety.
Early engagement with regulatory authorities allows researchers to align their development strategies with regulatory expectations, potentially avoiding costly missteps and delays. Pre-submission meetings and scientific advice procedures provide valuable guidance that can streamline the approval process.
Adaptive Clinical Trial Designs
Traditional clinical trial designs often lack the flexibility needed for efficient translational research. Adaptive trial designs allow modifications based on accumulating data, enabling researchers to optimize dosing, identify responsive patient subgroups, and make efficient use of limited resources.
These innovative approaches include basket trials testing single therapies across multiple diseases, umbrella trials evaluating multiple therapies for a single disease, and platform trials that can continuously add or remove treatment arms. Such designs accelerate the evaluation process while reducing costs and the number of patients needed.
Technology’s Transformative Role in Accelerating Translation 💻
Digital technologies and computational tools are revolutionizing translational research by enabling more efficient data collection, analysis, and integration. Artificial intelligence and machine learning algorithms can identify patterns in complex biological data, predict drug responses, and optimize clinical trial designs.
Electronic health records and real-world data sources provide unprecedented opportunities to evaluate treatment effectiveness in diverse patient populations outside controlled clinical trials. These data can identify promising therapeutic targets, validate biomarkers, and generate evidence supporting regulatory decisions.
Biobanks and data repositories facilitate access to biological samples and associated clinical information, enabling researchers to validate findings across multiple cohorts and accelerate the identification of clinically relevant discoveries. Standardized data sharing protocols enhance reproducibility and enable meta-analyses that strengthen evidence.
Digital Health Tools and Remote Monitoring
Wearable devices, mobile health applications, and remote monitoring technologies are transforming how researchers collect clinical data and engage with study participants. These tools enable continuous monitoring of patient outcomes, reduce the burden of in-person visits, and facilitate decentralized clinical trials that increase accessibility and diversity.
The COVID-19 pandemic accelerated adoption of these technologies, demonstrating their potential to maintain research momentum even during challenging circumstances. As regulatory agencies develop frameworks for incorporating digital endpoints, these tools will become increasingly central to translational research strategies.
Patient-Centered Approaches: Ensuring Relevant Impact 👥
Translational research must ultimately serve patient needs, making patient engagement essential throughout the research process. Incorporating patient perspectives from the earliest stages ensures that research priorities align with real-world needs and that study designs address questions most relevant to those who will use the resulting therapies.
Patient advocacy organizations have become powerful partners in translational research, providing funding, facilitating recruitment, and ensuring that research addresses community priorities. These partnerships have proven particularly valuable in rare disease research, where patient organizations often drive the translational agenda.
Patient-reported outcomes and quality-of-life measures provide critical data for evaluating treatment benefits beyond traditional clinical endpoints. Regulatory agencies increasingly recognize these measures as important evidence for approval decisions, particularly when objective endpoints are limited or not fully capture treatment impact.
Community Engagement and Health Equity
Ensuring that translational research benefits all populations requires intentional community engagement and attention to health equity. Historical underrepresentation of diverse populations in clinical research has resulted in treatments that may not work equally well for everyone.
Community-based participatory research approaches involve communities as equal partners in the research process, building trust and ensuring cultural appropriateness. These methods improve recruitment of underrepresented populations and generate findings more applicable to diverse real-world settings.
Entrepreneurship and Commercialization Strategies 💡
Successfully translating discoveries often requires entrepreneurial approaches and commercial partnerships. Academic researchers increasingly need business acumen to navigate intellectual property protection, licensing negotiations, and startup formation.
Technology transfer offices at academic institutions play crucial roles in protecting intellectual property, identifying commercial opportunities, and facilitating partnerships with industry. However, these offices must balance institutional interests with the urgency of getting treatments to patients.
Startup companies founded around academic discoveries can provide the focused resources and business expertise needed to advance development. However, these ventures require founding teams with complementary skills spanning science, business, and regulatory affairs.
Strategic Industry Partnerships
Partnerships with established pharmaceutical and biotechnology companies provide access to development expertise, manufacturing capabilities, and distribution networks that academic researchers lack. However, negotiating agreements that protect academic freedom while meeting industry needs requires careful navigation.
Different partnership models suit different situations, from sponsored research agreements and licensing deals to equity investments and joint ventures. Choosing the right model depends on development stage, intellectual property position, and strategic goals of all parties.
Education and Workforce Development: Preparing Translational Scientists 🎓
The interdisciplinary nature of translational research requires scientists with diverse skills spanning basic science, clinical research, regulatory affairs, and business development. Traditional training programs often fail to provide this breadth of expertise.
Specialized translational research training programs are emerging to address this gap, offering curricula that combine scientific rigor with practical skills in clinical trial design, regulatory strategy, and commercialization. These programs often include mentorship components connecting trainees with experienced translational researchers.
Career paths in translational research must be recognized and rewarded by academic institutions to attract talented researchers. Traditional academic metrics focused primarily on basic research publications may not adequately value the collaborative, applied nature of translational work.
Global Perspectives: International Collaboration and Knowledge Sharing 🌍
Many health challenges transcend national boundaries, requiring international collaboration to effectively translate discoveries into global impact. Diseases particularly affecting low- and middle-income countries often receive insufficient research attention despite high disease burden.
International research networks facilitate sharing of resources, data, and expertise while enabling studies in diverse populations that strengthen evidence generalizability. However, these collaborations must respect local contexts, build sustainable capacity, and ensure equitable benefit sharing.
Regulatory harmonization efforts aim to reduce duplication of requirements across countries, potentially accelerating global access to new therapies. While complete harmonization remains elusive, mutual recognition agreements and coordinated review processes are making progress.
Measuring Success: Defining Meaningful Outcomes
Evaluating translational research success requires metrics that capture the ultimate goal of improving health outcomes, not just academic productivity. Traditional measures like publications and citations, while important, do not adequately reflect translation into clinical practice.
Meaningful metrics might include patents filed, clinical trials initiated, regulatory approvals obtained, and ultimately, improvements in patient outcomes and healthcare delivery. However, the long timelines involved make real-time assessment challenging.
Institutions increasingly recognize the need for balanced scorecards that value both basic discovery and translational impact, creating incentive structures that encourage researchers to pursue both fundamental understanding and practical applications.
Overcoming Institutional Barriers and Cultural Shifts
Academic culture traditionally emphasizes individual achievement and disciplinary expertise, potentially hindering the collaborative, interdisciplinary approach translational research requires. Changing these cultural norms requires leadership commitment and structural changes to reward mechanisms.
Promotion and tenure criteria must recognize and value collaborative work, patents and licensing alongside publications, and engagement with industry and community partners. Without these changes, junior researchers may rationally avoid translational work that could jeopardize their careers.
Physical infrastructure also matters, with co-location of basic scientists, clinicians, and support services facilitating the spontaneous interactions and knowledge exchange that catalyze translational progress. Modern research buildings increasingly incorporate design features promoting cross-disciplinary collaboration.

Looking Forward: The Future of Translational Research 🚀
The translational research landscape continues evolving rapidly, driven by technological advances, policy changes, and growing recognition of the importance of accelerating impact. Emerging technologies like gene editing, personalized medicine, and regenerative therapies present both unprecedented opportunities and new translational challenges.
Artificial intelligence and big data analytics will increasingly enable identification of promising therapeutic targets and prediction of clinical outcomes before extensive human testing. However, these tools require careful validation and regulatory frameworks that balance innovation with safety.
The COVID-19 pandemic demonstrated what is possible when resources, regulatory flexibility, and collaborative urgency align around a common goal. The challenge now is sustaining these lessons and applying them to other health priorities without requiring a crisis to catalyze action.
Success in translational research ultimately requires systemic changes across multiple levels – from individual researcher training and institutional culture to funding mechanisms and regulatory frameworks. No single intervention will close the gap between laboratory discoveries and patient impact, but coordinated efforts across the ecosystem can dramatically accelerate progress.
By breaking down traditional barriers between disciplines, sectors, and stakeholders, we can create a more efficient translational pipeline that delivers on the promise of biomedical research: improving human health through scientific discovery. The tools, knowledge, and frameworks exist; what remains is the collective will to implement them systematically and sustain them over the long term required for transformative impact.
Toni Santos is a health systems analyst and methodological researcher specializing in the study of diagnostic precision, evidence synthesis protocols, and the structural delays embedded in public health infrastructure. Through an interdisciplinary and data-focused lens, Toni investigates how scientific evidence is measured, interpreted, and translated into policy — across institutions, funding cycles, and consensus-building processes. His work is grounded in a fascination with measurement not only as technical capacity, but as carriers of hidden assumptions. From unvalidated diagnostic thresholds to consensus gaps and resource allocation bias, Toni uncovers the structural and systemic barriers through which evidence struggles to influence health outcomes at scale. With a background in epidemiological methods and health policy analysis, Toni blends quantitative critique with institutional research to reveal how uncertainty is managed, consensus is delayed, and funding priorities encode scientific direction. As the creative mind behind Trivexono, Toni curates methodological analyses, evidence synthesis critiques, and policy interpretations that illuminate the systemic tensions between research production, medical agreement, and public health implementation. His work is a tribute to: The invisible constraints of Measurement Limitations in Diagnostics The slow mechanisms of Medical Consensus Formation and Delay The structural inertia of Public Health Adoption Delays The directional influence of Research Funding Patterns and Priorities Whether you're a health researcher, policy analyst, or curious observer of how science becomes practice, Toni invites you to explore the hidden mechanisms of evidence translation — one study, one guideline, one decision at a time.